No Results Found
The page you requested could not be found. Try refining your search, or use the navigation above to locate the post.
Primary tumors originating from the spine are very complex and challenging entities to
treat. Due to their rarity, a multicenter collaborative network is essential to shepherd the
best research and contribute to the dissemination of the best evidence possible. Over
the last few years, several advances have occurred in many different fields. Surgery is still
the cornerstone of treatment in most cases. The occasional suboptimal outcomes and
high morbidity of surgical treatment have however encouraged professionals caring for
these patients to explore safer treatment options and alternatives or adjuncts to surgical
treatment. A number of novel treatment strategies have emerged from the medical, interventional radiology, radiation oncology, and molecular worlds. This has truly positioned
primary spine tumors at the forefront of multidisciplinary care. This article discusses these
recent advances in detail to equip the oncologic spine surgeon and their team to better
counsel and treat these patients. Most of these advances allow for a more tailored, efficient,
and, most importantly, less morbid management of primary spine tumors. Some of these
advances are still under investigation, however, and evidence-based oncological principles
should still be strongly encouraged.
Non-mechanical back pain, especially in the middle or lower back, is the most frequent symptom of both benign and malignant spinal tumors. This back pain is not specifically attributed to injury, stress or physical activity. However, the pain may increase with activity and is often worse at night. Pain may spread beyond the back to the hips, legs, feet or arms and may worsen over time — even when treated by conservative, nonsurgical methods that can often help alleviate back pain attributed to mechanical causes. Depending on the location and type of tumor, other signs and symptoms can develop, especially as a malignant tumor grows and compresses on the spinal cord, the nerve roots, blood vessels or bones of the spine. Impingement of the tumor on the spinal cord can be life-threatening in itself.
Additional symptoms can include the following:
Loss of sensation or muscle weakness in the legs, arms or chest
Difficulty walking, which may cause falls
Decreased sensitivity to pain, heat and cold
Loss of bowel or bladder function
Paralysis that may occur in varying degrees and in different parts of the body, depending on which nerves are compressed
Scoliosis or other spinal deformity resulting from a large, but benign tumor
A thorough medical examination with emphasis on back pain and neurological deficits is the first step to diagnosing a spinal tumor. Radiological tests are required for an accurate and positive diagnosis.
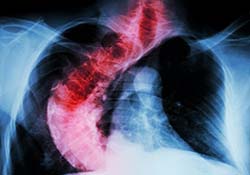
X-ray: Application of radiation to produce a film or picture of a part of the body can show the structure of the vertebrae and the outline of the joints. X-rays of the spine are obtained to search for other potential causes of pain, i.e. tumors, infections, fractures, etc. X-rays are not very reliable in diagnosing tumors.
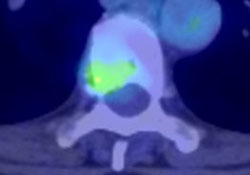
Computed tomography scan (CT or CAT scan): A diagnostic image created after a computer reads X-rays, a CT/CAT scan can show the shape and size of the spinal canal, its contents and the structures around it. It also is very good at visualizing bony structures.
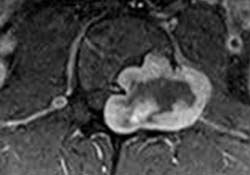
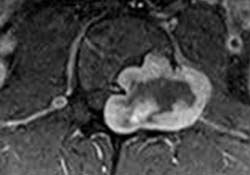
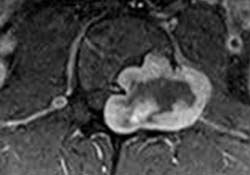
Magnetic resonance imaging (MRI): A diagnostic test that produces three-dimensional images of body structures using powerful magnets and computer technology. An MRI can show the spinal cord, nerve roots and surrounding areas, as well as enlargement, degeneration and tumors.
After radiological confirmation of the tumor, the only way to determine whether the tumor is benign or malignant is to examine a small tissue sample (extracted through a biopsy procedure) under a microscope. If the tumor is malignant, a biopsy also helps determine the cancer’s type, which subsequently determines treatment options.
Staging classifies neoplasms (abnormal tissue) according to the extent of the tumor, assessing bony, soft tissue and spinal canal involvement. A doctor may order a whole body scan utilizing nuclear technology, as well as a CT scan of the lungs and abdomen for staging purposes. To confirm diagnosis, a doctor compares laboratory test results and findings from the aforementioned scans to the patient’s symptoms.
Treatment Decisions
Treatment decision-making is often multidisciplinary, incorporating the expertise of spinal surgeons, medical oncologists, radiation oncologists and other medical specialists. The selection of treatments including both surgical and non-surgical is therefore made keeping in mind the various aspects of the patient’s overall health and goals of care.
Nonsurgical treatment options include observation, chemotherapy and radiation therapy. Tumors that are asymptomatic or mildly symptomatic and do not appear to be changing or progressing may be observed and monitored with regular MRIs. Some tumors respond well to chemotherapy and others to radiation therapy. However, there are specific types of metastatic tumors that are inherently radioresistant (i.e. chordoma and chondrosarcoma): in those cases, surgery may be the only viable treatment option.
Indications for surgery vary depending on the type of tumor. Primary spinal tumors may be removed through complete piecemeal (benign tumors) or en bloc (malignant tumors) resection for a possible cure. Indication, planning and performing of the surgery in case of a primary spinal tumor is one of the most complex and challenging fields of spine surgery.
For cases in which surgical resection is possible, preoperative embolization may be used to enable an easier resection. This procedure involves the insertion of a catheter or tube through an artery in the groin. The catheter is guided up through the blood vessels to the site of the tumor, where it delivers a glue-like liquid embolic agent that blocks the vessels that feed the tumor. When the blood vessels that feed the tumor are blocked off, bleeding can often be controlled better during surgery, helping to decrease surgical risks.
The posterior (back) approach allows for the identification of the dura and exposure of the nerve roots. Multiple levels can be decompressed, and multilevel segmental fixation can be performed. The anterior (front) approach is excellent for tumors in the front of the spine and effectively reconstructing defects caused by removal of the vertebral bodies. This approach also allows placement of short-segment fixation devices. Thoracic and lumbar spinal tumors that affect both the anterior and posterior vertebral columns can be a challenge to resect completely. Not infrequently, a posterior (back) approach followed by a separately staged anterior (front) approach has been utilized surgically to treat these complex lesions.
The typical hospital stay after surgery to remove a spinal tumor ranges from 2 to 14 days, depending on the patient’s case. A required period of post-surgery physical rehabilitation may involve a stay in a rehabilitation hospital for a period of time. In other cases, physical therapy may take place at an outpatient facility or at the patient’s home. The total recovery time after surgery may be as short as three months or as long as one year, depending on the complexity of the surgery and the patient’s overall health.
Outcome depends greatly on the type of the tumor, age and overall health of the patient. In the case of metastatic tumors, the goal is almost always curative, with treatment aimed at providing the patient with an improved quality of life and disease free survival.
(aans.org)
The page you requested could not be found. Try refining your search, or use the navigation above to locate the post.

The spinal column is the most common site for bone metastasis. Estimates indicate that at least 30 percent and as high as 70 percent of patients with cancer will experience spread of cancer to their spine.
Common primary cancers that spread to the spine are lung, breast and prostate. Lung cancer is the most common cancer to metastasize to the bone in men, and breast cancer is the most common in women. Other cancers that spread to the spine include multiple myeloma, lymphoma, melanoma and sarcoma, as well as cancers of the gastrointestinal tract, kidney and thyroid. Prompt diagnosis and identification of the primary malignancy is crucial to overall treatment. Numerous factors can affect outcome, including the nature of the primary cancer, the number of lesions, the presence of distant non-skeletal metastases and the presence and/or severity of spinal-cord compression.
Non-mechanical back pain, especially in the middle or lower back, is the most frequent symptom of both benign and malignant spinal tumors. This back pain is not specifically attributed to injury, stress or physical activity. However, the pain may increase with activity and is often worse at night. Pain may spread beyond the back to the hips, legs, feet or arms and may worsen over time — even when treated by conservative, nonsurgical methods that can often help alleviate back pain attributed to mechanical causes. Depending on the location and type of tumor, other signs and symptoms can develop, especially as a malignant tumor grows and compresses on the spinal cord, the nerve roots, blood vessels or bones of the spine. Impingement of the tumor on the spinal cord can be life-threatening in itself.
Additional symptoms can include the following:
Loss of sensation or muscle weakness in the legs, arms or chest
Difficulty walking, which may cause falls
Decreased sensitivity to pain, heat and cold
Loss of bowel or bladder function
Paralysis that may occur in varying degrees and in different parts of the body, depending on which nerves are compressed
Scoliosis or other spinal deformity resulting from a large, but benign tumor
A thorough medical examination with emphasis on back pain and neurological deficits is the first step to diagnosing a spinal tumor. Radiological tests are required for an accurate and positive diagnosis.
X-ray: Application of radiation to produce a film or picture of a part of the body can show the structure of the vertebrae and the outline of the joints. X-rays of the spine are obtained to search for other potential causes of pain, i.e. tumors, infections, fractures, etc. X-rays are not very reliable in diagnosing tumors.
Computed tomography scan (CT or CAT scan): A diagnostic image created after a computer reads X-rays, a CT/CAT scan can show the shape and size of the spinal canal, its contents and the structures around it. It also is very good at visualizing bony structures.
Magnetic resonance imaging (MRI): A diagnostic test that produces three-dimensional images of body structures using powerful magnets and computer technology. An MRI can show the spinal cord, nerve roots and surrounding areas, as well as enlargement, degeneration and tumors.
After radiological confirmation of the tumor, the only way to determine whether the tumor is benign or malignant is to examine a small tissue sample (extracted through a biopsy procedure) under a microscope. If the tumor is malignant, a biopsy also helps determine the cancer’s type, which subsequently determines treatment options.
Staging classifies neoplasms (abnormal tissue) according to the extent of the tumor, assessing bony, soft tissue and spinal canal involvement. A doctor may order a whole body scan utilizing nuclear technology, as well as a CT scan of the lungs and abdomen for staging purposes. To confirm diagnosis, a doctor compares laboratory test results and findings from the aforementioned scans to the patient’s symptoms.
Treatment Decisions
Treatment decision-making is often multidisciplinary, incorporating the expertise of spinal surgeons, medical oncologists, radiation oncologists and other medical specialists. The selection of treatments including both surgical and non-surgical is therefore made keeping in mind the various aspects of the patient’s overall health and goals of care.
Nonsurgical treatment options include observation, chemotherapy and radiation therapy. Tumors that are asymptomatic or mildly symptomatic and do not appear to be changing or progressing may be observed and monitored with regular MRIs. Some tumors respond well to chemotherapy and others to radiation therapy. However, there are specific types of metastatic tumors that are inherently radioresistant (i.e. gastrointestinal tract and kidney): in those cases, surgery may be the only viable treatment option.
Indications for surgery vary depending on the type of tumor. In patients with metastatic tumors, treatment is primarily palliative, with the goal of restoring or preserving neurological function, stabilizing the spine and alleviating pain. Generally, surgery is only considered as an option for patients with metastases when they are expected to live 12 weeks or longer, and the tumor is resistant to radiation or chemotherapy. Indications for surgery include intractable pain, spinal-cord compression and the need for stabilization of impending pathological fractures.
For cases in which surgical resection is possible, preoperative embolization may be used to enable an easier resection. This procedure involves the insertion of a catheter or tube through an artery in the groin. The catheter is guided up through the blood vessels to the site of the tumor, where it delivers a glue-like liquid embolic agent that blocks the vessels that feed the tumor. When the blood vessels that feed the tumor are blocked off, bleeding can often be controlled better during surgery, helping to decrease surgical risks.
The posterior (back) approach allows for the identification of the dura and exposure of the nerve roots. Multiple levels can be decompressed, and multilevel segmental fixation can be performed. The anterior (front) approach is excellent for tumors in the front of the spine and effectively reconstructing defects caused by removal of the vertebral bodies. This approach also allows placement of short-segment fixation devices. Thoracic and lumbar spinal tumors that affect both the anterior and posterior vertebral columns can be a challenge to resect completely. Not infrequently, a posterior (back) approach followed by a separately staged anterior (front) approach has been utilized surgically to treat these complex lesions.
The typical hospital stay after surgery to remove a spinal tumor ranges from 2 to 14 days, depending on the patient’s case. A required period of post-surgery physical rehabilitation may involve a stay in a rehabilitation hospital for a period of time. In other cases, physical therapy may take place at an outpatient facility or at the patient’s home. The total recovery time after surgery may be as short as three months or as long as one year, depending on the complexity of the surgery and the patient’s overall health.
Outcome depends greatly on the age and overall health of the patient. In the case of metastatic tumors, the goal is almost always palliative, with treatment aimed at providing the patient with an improved quality of life and possibly prolonged life expectancy.
(aans.org)
The page you requested could not be found. Try refining your search, or use the navigation above to locate the post.
Increasing number of people are suffering from a spine tumor. While primary tumors are rare conditions, metastatic lesions (a distant secondary tumor of a primary cancer) are more frequent due to the population aging and extended survival of cancer patients. These tumors can cause severe pain, neurological deficit and a significant decrease of quality of life. Due to the development of spine surgical techniques and also the modern radiotherapy, most of the spinal tumors can be succesfully treated providing a pain relief and improvement of the patient’s quality of life. The emergence of minimally invasive surgical techniques have widen the group of surgically manageable patients. Because of the severity of the disease and the complexity of the therapy, spine tumor surgeries can be performed effectively and safely only by experienced spine surgeons in spine tumor centers.
These tumors are rare diseases where surgical treatment is often the only one therapeutic option.

Secondary spinal cancer is a frequent, painful and disabling condition, where surgery can improve the quality of life.

World-wide leader group of international spine tumor experts – including Dr. Lazary – performs high quality research.
The page you requested could not be found. Try refining your search, or use the navigation above to locate the post.

Back pain is one of the most common symptoms in human life. It is a spectrum, a multifactorial condition. Back pain can be originated from functional causes (such as muscle spasms) to very severe diseases (such as a spinal tumor). Therefore, the proper diagnosis and the management of a patient with back pain is crucial. Most of the back pain conditions do not require a surgical intervention, but there are several cases when surgical treatment can provide pain relief, complete healing and functional improvement. The key element of the successful treatment is the detailed diagnostic process and the perfect application of the appropriate surgical method. The decision making process is often personalized requiring evidence based, modern decision supporting tools.

Disc herniation is a common problem where the indication and the timing of the surgical intervention is crucial.

In case of a disabling spinal stenosis, pain relief and functional restoration can be achieved with surgery.

Segmental instability can result in loss of quality of life and working ability when surgical stabilization is indicated.
Progrediating spinal deformity is a painful condition where only the surgical correction can cure the patient.

Most of the traumatic or compression fractures can be treated with minimal invasive methods providing pain relief.
In patients suffered from a spine tumor, quality of life influenced by pain is in the focus of the treatment process.

Personal information:
Name Aron Lazary MD PhD
Nationality Hungarian
E-mail aron.lazary@bhc.hu
Office: Kiralyhago u. 1-3., Budapest, Hungary, H-1126
Employment history:
2018-: National Center for Spinal Disorders – Deputy Director
2016-: Semmelweis University, Department of Musculoskeletal Oncology – board member
2014-: National Center for Spinal Disorders – Scientific Director, spine surgeon
2008-2014: National Center for Spinal Disorders – Head of R&D, resident
2012-: Semmelweis University Doctoral School – PhD supervisor and lecturer
2005-2008: Semmelweis University, 1st Department of Medicine, Molecular Genetics Laboratory – PhD student
Education:
2011- Spine surgery courses, fellowships (AOSpine, Eurospine)
2008-2014: Semmelweis University and National Center for Spinal Disorders (orthopeadics-traumatology board exam, 2014)
2005-2010: Semmelweis University, Doctoral School (PhD, 2010)
1999-2005: Semmelweis University, Medical School (MD, 2005)
1995-1999: ELTE Apáczai Cs. János Secondary School
Awards and fellowships:
2017: EMSOS 2017, „Best oral presentation”
2014: TOP25 Hungarian young medical scientists
2014: Eurospine 2014, „Best of show” abstract
2013: Eurospine 2013, „Best of show” abstract
2012: Eurospine 2012, Travel Grant
2012: Zinner Award of the Hungarian Orthopaedic Society
2010: Eurospine 2010, „Best of show” abstract
2008: Junior Prima Prize in Hungarian Science Category
Grants
2018- SPINNER (Horizon2020 Marie-Curie Action, 77k EUR)
2017- OTKA FK23884 (Principal Investigator, 120k EUR)
2016- AOSpine PTRON (Co-Investigator)
2014-2018 AOSpine EPOSO (Co-Investigator)
2012-2015 OTKA PD104604 (Principal Investigator, 46k EUR)
2012-2015 Eurospine Task Force on Research (Co-Investigator, 30k EUR)
2011-2012 AOSpine PT retro (Co-Investigator, 18k EUR)
2011-2012 AOSpine SINS (Coordinator)
2011-2014 „MySpine” FP7 HEALTH-F2-2008-269909 (Co-Investigator, 300k EUR)
2008-2013 „Genodisc” FP7 HEALTH-F2-2008-201626 (Co-Investigator, 200k EUR)
Clinical trial experience
2017- STRIVE (Co-Investigator)
2016-2017 REGN475 (Principal Investigator)
2011-2015 APOLLO (Co-Investigator, Site-Coordinator)
2011-2015 APPROACH-001-EU (Co-Investigator, Site-Coordinator)
2009-2013 PRESTIGE Observational Study (Sub-Investigator)
2008-2011 ACADIA 1020-9061 (Site-Coordinator)
Publications:
Papers in international journals: 54
Papers in Hungarian journals: 30
Impact factor: 132.78
Citations: 610 (Researchgate)
h-index: 11
Editorial experience:
Hungarian Spine Journal (2014-, Editor)
International Journal of Orthopedics and Rehabilitation (2014-, member of Editorial Board)
European Spine Journal (2013-, reviewer, 2015 – Assitant Editor)
Global Spine Journal (2012-, reviewer)
Evidence Based Spine Journal (2011, reviewer)
Professional memberships:
Eurospine (National Contact Person)
AOSpine, AOSpine Hungary Chairperson (2015-), Member of the European Research Committee (2010—13), AOSpine Knowledge Forum Tumors (Associate Member)
Hungarian Orthopaedic Society
Hungarian Spine Society
Educational activity
2018- European Spine Diploma (international faculty)
2015- Semmelweis University, Faculty of Medicine, Department of Anatomy (invited lecturer)
2011- AOSpine Courses (faculty/chairperson)
2011- Semmelweis University, Doctoral School (PhD supervisor)
Peer reviewed publications:
Lazáry Á, Szövérfi Z, Varga PP. [Change of the paradigm in the surgical treatment of metastatic diseases of bone Part II. Treatment of spinal metastases.] Orv Hetil. 2018, accepted manuscript (IF: 0.349)
Szendrői M, Antal I, Szendrői A, Lazáry Á, Varga PP. Diagnostic algorithm, prognostic factors and surgical treatment of metastatic cancer diseases of the long bones and spine. EFORT Open Rev. 2017 Sep 1;2(9):372-381. doi: 10.1302/2058-5241.2.170006. eCollection 2017 Sep. Review.
Fortin M, Lazáry À, Varga PP, Battié MC. Association between paraspinal muscle morphology, clinical symptoms and functional status in patients with lumbar spinal stenosis. Eur Spine J. 2017 Oct;26(10):2543-2551. doi: 10.1007/s00586-017-5228-y. Epub 2017 Jul 26. (IF: 2.563)
Horváth E, Balla B, Kósa J, Lakatos PA, Lazáry Á, Németh D, Jozilan H, Somorácz Á, Korompay A, Gyöngyösi B, Borka K, Kiss A, Kupcsulik P, Schaff Z, Szalay F. [Vitamin D metabolism and signaling in human hepatocellular carcinoma and surrounding non-tumorous liver] Orv Hetil. 2016 Nov;157(48):1910-1918. Hungarian. (IF: 0.349)
Dea N, Charest-Morin R, Sciubba DM, Bird JE, Disch AC, Mesfin A, Lazáry Á, Fisher CG, Ames C. Optimizing the Adverse Event and HRQOL Profiles in the Management of Primary Spine Tumors. Spine (Phila Pa 1976). 2016 Oct 15;41 Suppl 20:S212-S217. (IF: 2.439)
Laufer I, Zuckerman SL, Bird JE, Bilsky MH, Lazáry Á, Quraishi NA, Fehlings MG, Sciubba DM, Shin JH, Mesfin A, Sahgal A, Fisher CG. Predicting Neurologic Recovery after Surgery in Patients with Deficits Secondary to MESCC: Systematic Review. Spine (Phila Pa 1976). 2016 Oct 15;41 Suppl 20:S224-S230. (IF: 2.439)
Bettegowda C, Yip S, Lo SL, Fisher CG, Boriani S, Rhines LD, Wang JY, Lazary A, Gambarotti M, Wang WL, Luzzati A, Dekutoski MB, Bilsky MH, Chou D, Fehlings MG, McCarthy EF, Quraishi NA, Reynolds JJ, Sciubba DM, Williams RP, Wolinsky JP, Zadnik PL, Zhang M, Germscheid NM, Kalampoki V, Varga PP, Gokaslan ZL; AOSpine Knowledge Forum Tumor. Spinal column chordoma: prognostic significance of clinical variables and T (brachyury) gene SNP rs2305089 for local recurrence and overall survival. Neuro Oncol. 2016 Sep 23. pii: now156. [Epub ahead of print] (IF: 7.371)
Klemencsics I, Lazary A*, Szoverfi Z, Bozsodi A, Eltes P, Varga PP. Risk factors for surgical site infection in elective routine degenerative lumbar surgeries. Spine J. 2016 Aug 9. pii: S1529-9430(16)30869-5. doi: 10.1016/j.spinee.2016.08.018. (IF: 2.660)
Castro-Mateos I, Hua R, Pozo JM, Lazary A, Frangi AF. Intervertebral disc classification by its degree of degeneration from T2-weighted magnetic resonance images. Eur Spine J. 2016 Sep;25(9):2721-7. doi: 10.1007/s00586-016-4654-6 (IF: 2.132)
Fortin M, Lazáry À, Varga PP, McCall I, Battié MC. Paraspinal muscle asymmetry and fat infiltration in patients with symptomatic disc herniation. Eur Spine J. 2016 May;25(5):1452-9. doi: 10.1007/s00586-016-4503-7. (IF: 2.132)
Bozsodi A, Boja S, Szilagyi A, Somhegyi A, Varga PP, Lazary A*. Muscle strength is associated with vitamin D receptor gene variants. J Orthop Res. 2016 Mar 2. doi: 10.1002/jor.23220. [Epub ahead of print] (IF: 2.807)
Valasek T, Varga PP, Klemencsics I, Szövérfi Z, Bozsódi Á, Éltes PE, Lazáry Á*. [MEASURING THE FUNCTIONAL IMPAIRMENT OF THE LUMBAR SPINE]. Ideggyogy Sz. 2015 Mar 30;68(3-4):135-41. Hungarian. (IF: 0.376)
Castro-Mateos I, Pozo JM, Pereañez M, Lekadir K, Lazary A, Frangi AF. Statistical Interspace Models (SIMs): Application to Robust 3D Spine Segmentation. IEEE Trans Med Imaging. 2015 Aug;34(8):1663-75. doi: 10.1109/TMI.2015.2443912. Epub 2015 Jun 11. (IF: 3.756)
Varga PP, Jakab G, Bors IB, Lazary A, Szövérfi Z. Experiences with PMMA cement as a stand-alone intervertebral spacer : Percutaneous cement discoplasty in the case of vacuum phenomenon within lumbar intervertebral discs. English Version. Orthopade. 2015 Feb;44(2):124-31. doi: 10.1007/s00132-015-3092-1. German. (IF: 0.373)
Pereanez M, Lekadir K, Castro-Mateos I, Pozo J, Lazary A, Frangi A. Accurate Segmentation of Vertebral Bodies and Processes using Statistical Shape Decomposition and Conditional Models. IEEE Trans Med Imaging. 2015 Jan 27. [Epub ahead of print] (IF: 3.799)
Klemencsics I, Lazary A*, Valasek T, Szoverfi Z, Bozsodi A, Eltes P, Fekete TF, Varga PP. Cross-cultural adaptation and validation of the Hungarian version of the Core Outcome Measures Index for the back (COMI Back). Eur Spine J. 2015 Jan 9. [Epub ahead of print] (IF: 2.132)
Varga PP, Szövérfi Z, Fisher CG, Boriani S, Gokaslan ZL, Dekutoski MB, Chou D, Quraishi NA, Reynolds JJ, Luzzati A, Williams R, Fehlings MG, Germscheid NM, Lazary A, Rhines LD. Surgical treatment of sacral chordoma: prognostic variables for local recurrence and overall survival. Eur Spine J. 2015 May;24(5):1092-101. doi: 10.1007/s00586-014-3728-6. Epub 2014 Dec 23. (IF: 2.132)
Castro-Mateos I, Pozo JM, Eltes PE, Rio LD, Lazary A, Frangi AF. 3D segmentation of annulus fibrosus and nucleus pulposus from T2-weighted magnetic resonance images. Phys Med Biol. 2014 Nov 24;59(24):7847-7864. (IF: 2.922)
Lazary A. Commentary on: “L4 and L5 Spondylectomy for En Bloc Resection of Giant Cell Tumor and Review of the Literature”. Evid Based Spine Care J. 2014 Oct;5(2):158-9. doi: 10.1055/s-0034-1387801.
Neidlinger-Wilke C, Boldt A, Brochhausen C, Galbusera F, Carstens C Prof, Copf F, Schulthei M, Lazary A, Brayda-Bruno M, Ignatius A Prof Dr, Wilke HJ Prof Dr. Molecular Interactions Between Human Cartilaginous Endplates and Nucleus Pulposus Cells: A Preliminary Investigation. Spine (Phila Pa 1976). 2014 May 14. [Epub ahead of print] (IF: 2.159)
Szövérfi Z, Lazáry A, Varga PP. [Primary spinal tumor registry in the national centre for spinal disorders]. Orv Hetil. 2014 May 1;155(19):745-9. doi: 10.1556/OH.2014.29920. Hungarian.
Varga PP, Szoverfi Z, Lazary A*. Surgical resection and reconstruction after resection of tumors involving the sacropelvic region. Neurol Res. 2014 Apr 27:1743132814Y0000000370. (IF: 1.182)
Varga PP, Szövérfi Z, Lazary A. Surgical treatment of primary malignant tumors of the sacrum. Neurol Res. 2014 Apr 27:1743132814Y0000000366. (IF: 1.182)
Valasek T, Varga PP, Szövérfi Z, Bozsodi A, Klemencsics I, Fekete L, Lazary A*. Validation of the Hungarian version of the Roland-Morris disability questionnaire. Disabil Rehabil. 2014 Apr 21. (IF: 1.541)
Szövérfi Z – Lazáry A, Bozsódi A, Klemencsics I, Eltes P, Varga PP. Primary Spinal Tumor Mortality Score (PSTMS): a novel scoring system for predicting poor survival. Spine J. 2014 Mar 17. pii: S1529-9430(14)00250-2. doi: 10.1016/j.spinee.2014.03.009. (IF: 3.355)
Lazary A, Szövérfi Z, Szita J, Somhegyi A, Kümin M, Varga PP. Primary prevention of disc degeneration-related symptoms. Eur Spine J. 2013 Nov 13. [Epub ahead of print] (IF: 2.133)
Scheipl S, Lohberger B, Rinner B, Froehlich EV, Beham A, Quehenberger F, Lazáry A, Pal Varga P, Haybaeck J, Leithner A, Liegl B. Histone deacetylase inhibitors as potential therapeutic approaches for chordoma: an immunohistochemical and functional analysis. J Orthop Res. 2013 Dec;31(12):1999-2005. doi: 10.1002/jor.22447. Epub 2013 Jul 24. (IF: 2.875)
Battié MC, Lazáry A, Fairbank J, Eisenstein S, Heywood C, Brayda-Bruno M, Varga PP, McCall I. Disc degeneration-related clinical phenotypes. Eur Spine J. 2013 Jul 25. [Epub ahead of print] (IF: 2.133)
Sivan SS, Merkher Y, Wachtel E, Urban JP, Lazary A, Maroudas A. A needle micro-osmometer for determination of glycosaminoglycan concentration in excised nucleus pulposus tissue. Eur Spine J. 2013 Aug;22(8):1765-73. doi: 10.1007/s00586-013-2714-8. Epub 2013 Feb 18. (IF: 2.133)
Valasek T, Varga PP, Szövérfi Z, Kümin M, Fairbank J, Lazary A*. Reliability and validity study on the Hungarian versions of the Oswestry Disability Index and the Quebec Back Pain Disability Scale. Eur Spine J. 2013 Jan 16. [Epub ahead of print] (IF: 2.133)
Ben Mansour K, Dao TT, Charleux F, Lazáry A, Varga PP, Ho Ba Tho MC, Marin F. A non invasive protocol for the in vivo estimation of lumbar spine kinematics. Comput Methods Biomech Biomed Engin. 2012;15 Suppl 1:200-2. No abstract available.
Sivan SS, Van El B, Merkher Y, Schmelzer CE, Zuurmond AM, Heinz A, Wachtel E, Varga PP, Lazary A, Brayda-Bruno M, Maroudas A. Longevity of elastin in human intervertebral disc as probed by the racemization of aspartic acid. Biochim Biophys Acta. 2012 Oct;1820(10):1671-7. Epub 2012 Jun 21.(IF: 5.000)
Lazáry A, Bors IB, Szövérfi Z, Rónai M, Varga PP. [Prognostic factors of primary spinal tumors]. Ideggyogy Sz. 2012 May 30;65(5-6):161-7. Hungarian. (IF: 0.35)
Lazáry A, Ito K, Eisenstein S, Fairbank J, Roberts S, Kletsas D, Kümin M, Brayda-Bruno M, Varga PP. Surgeons and scientists: symbiosis in spinal research? Eur Spine J. 2012 Jun 1.Scheipl S, Froehlich EV, Leithner A, Beham A, Quehenberger F, Mokry M, Stammberger H, Varga PP, Lazáry A, Windhager R, Gattenloehner S, Liegl B. Does insulin-like growth factor 1 receptor (IGF-1R) targeting provide new treatment options for chordomas? A retrospective clinical and immunohistochemical study. Histopathology. 2012 May;60(6):999-1003. (IF: 3.082)Balla B, Vaszilko M, Kósa J, Podani J, Takács I, Tóbiás B, Nagy Z, Lazáry A, Lakatos P. New approach to analyze genetic and clinical data in bisphosphonate-induced osteonecrosis of the jaw. Oral Dis. 2012 Jan 31. doi: 10.1111/j.1601-0825.2012.01912.x. [Epub ahead of print] (IF: 2.495)Froelich EV, Scheipl S, Lazary A, Varga PP, Schmid C, Stammberger H, Beham A, Bodo K, Schroettner H, Quehenberger F, Windhager R, Liegl B, Leithner A. Expression of Ezrin, Mmp-9 and Cox-2 in 50 Chordoma Specimens: A Clinical and Immunohistochemical Analysis. Spine (Phila Pa 1976). 2012 Jan 5. [Epub ahead of print] (IF: 2,078)
Kiss J, Balla B, Kósa JP, Borsy A, Podani J, Takács I, Lazáry A, Nagy Z, Bácsi K, Kis A, Szlávy E, Szendrői M, Speer G, Orosz L, Lakatos P. Gene expression patterns in the bone tissue of women with fibrous dysplasia. Am J Med Genet A. 2010 Aug 3. (IF: 2,404)
Varga PP, Lazary A. Chordoma of the sacrum: “en bloc” high partial sacrectomy. Eur Spine J. 2010 Jun;19(6):1037-8. (IF:1.956)
Varga PP, Lazary A. Chordoma of the sacrum: “en bloc” total sacrectomy and lumbopelvic reconstruction. Eur Spine J. 2010 Jun;19(6):1039-40. (1.956)
Takacs I – Lazary A, Kosa J, Kiss J, Balla B, Nagy Z, Bacsi K, Speer G, Lakatos P: Allelic variations of RANKL/OPG signaling system is related to bone mineral density and in vivo gene expression. Eur J Endocrinol. 2009 Nov 24. (IF: 3,539)
Kósa JP, Balla B, Kiss J, Podani J, Takács I, Lazáry A, Nagy Z, Bácsi K, Karsai A, Speer G, Lakatos P. Postmenopausal expression changes of immune system-related genes in human bone tissue. J Clin Immunol. 2009 Nov;29(6):761 (IF: 3,583)
Balla B, Kósa JP, Kiss J, Podani J, Takács I, Lazáry Á, Nagy Zs, Bácsi K, Speer G, Lakatos P: Transcriptional profiling of immune system-related genes in postmenopausal osteoporotic versus non-osteoporotic human bone tissue. Clinical Immunology – 2009 Feb 19. (IF: 3,863)
Lazary J, Lazary A, Gonda X, Benkő A, Molnár E, Juhász G, Bagdy G: Promoter variants of the cannabinoid receptor 1 gene (CNR1) in interaction with 5-HTTLPR affect the anxious phenotype. Am J Med Genet B Neuropsychiatr Genet. 2009 Sep 1. (IF: 3,481)
Bácsi K, Kósa JP, Lazáry A, Balla B, Horváth H, Kis A, Nagy Z, Takács I, Lakatos P, Speer G: LCT 13910 C/T polymorphism, serum calcium, and bone mineral density in postmenopausal women. Osteoporos Int. 2009 Apr;20(4):639-45. (IF: 4,997)
Varga PP, Bors IB, Lazary Á: Sacral tumors and Management, Orthopaedic Clinics of North America 2009 Jan; 40(1):105-123. (IF: 1,245)
Kosa JP, Balla B, Kiss J, Borsy A, Podani J, Takács I, Lazáry Á, Nagy Zs, Bácsi K, Speer G, Orosz L, Lakatos P: Effect of menopause on gene expression pattern in bone tissue of non-osteoporotic women, Menopause (2009), vol. 16(2) pp 367-377 (IF: 3,082)
Bacsi K, Hitre E, Kosa JP, Horvath H, Lazary A, Lakatos PL, Balla B, Budai B, Lakatos P, Speer G: Effects of the lactase 13910 C/T and calcium-sensor receptor A986S G/T gene polymorphisms on the incidence and recurrence of colorectal cancer in Hungarian population, BMC Cancer 2008 Nov 3;8:317 (IF: 2,71)
Lazary J, Lazary A, Gonda X, Benkő A, Molnár E, Juhász G, Bagdy G: New evidence for the association of the serotonin transporter gene (SLC6A4) haplotypes, threatening life events and depressive phenotype, Biological Psychiatry 2008 Sep 15;64(/):498-504 (IF: 8,456)
Lazáry Á – Kósa JP, Tóbiás B, Balla B, Bácsi B, , Nagy Zs, Takács I, Mező T, Speer G, Lakatos P: Single nucleotide polymorphisms in new candidate genes are associated with bone mineral density and fracture risk, European Journal of Endocrinology 2008 Aug;159(2):187-96. (IF: 3,239)
Lazáry Á – Speer G, Varga PP, Balla B, Bácsi B, Kósa JP, Nagy Zs, Takács I, Lakatos P: The effect of vertebroplasty filler materials on viability and gene expression of human nucleus pulposus cells, Journal of Orthopaedic Research 2008 Jan 4. (IF: 2,437)
Balla B, Kósa JP, Kiss J, Borsy A, Podani J, Takács I, Lazáry Á, Nagy Zs, Bácsi K, Speer G, Orosz L, Lakatos P: Different Gene Expression Patterns in the Bone Tissue of Aging Postmenopausal Osteoporotic and Non-osteoporotic Women Calcified Tissue International 2008 Jan;82(1):12-26. (IF: 2,435)
Bácsi K, Borgulya G, Kósa JP, Lazáry Á, Balla B, Nagy Zs, Takács I, Speer G, Lakatos P: CYP3A7*1 polymorphism, serum dehydroepiandosterone sulphate level and bone mineral density in postmenopausal women, Calcified Tissue International 2007 Mar; 80:154-159. (IF:2,435)
Lazáry Á, Balla B, Kósa JP, Bácsi K, Nagy Zs, Takács I, Varga PP, Speer G, Lakatos P: Effect of gypsum on proliferation and differentiation of MC3T3-E1 mouse osteoblastic cells, Biomaterials, 2007 Jan;28(3):393-9. (IF: 6,262)
Lazáry A, Bors IB, Szövérfi Zs, Rónai M, Varga PP: Primer gerinctumorok prognosztikai faktorai [Prognostic factors of primary spine tumors ]. Ideggyógyászati szemle, 2012 May 30;65(5-6):161-7. (IF: 0,488)
Varga PP, Bors IB, Lazáry Á. Orthopedic treatment of vertebral compression fractures in osteoporosis. Orv Hetil. 2011 Aug 14;152(33):1328-36. Review. Hungarian.
Kiss J, Balla B, Kósa PJ, Borsy A, Podani J, Takács I, Lazáry A, Nagy Z, Bácsi K, Szlávy E, Szendrôi M, Speer G, Orosz L, Lakatos P. Changes of gene expression and its role in pathogenesis in fibrous and non-fibrous dysplastic bone tissues in women. Orv Hetil. 2010 Oct 3;151(40):1656-65. Hungarian.
Lazáry Á, Balla B, Bácsi K, Kósa JP, Nagy Zs, Takács I, Speer G, Varga PP, Lakatos P: A szintetikus csontpótló graftok alkalmazásának összefoglalása. A gipsz szerepe a csontpótlásban: molekuláris biológiai megközelítéssel, saját eredményeink alapján, Orvosi Hetilap – 2007 Dec (148) 51.2427-2433.
Bácsi K, Kósa JP, Lazáry Á, Horváth H, Balla B, Lakatos P, Speer G: A dehidroepiandroszteron és dehidroepiandroszteron szulfát jelentősége a különböző kórállapotokban. Saját eredmények és irodalmi adatok összefoglalása, Orvosi Hetilap 2007;148(14):651-7.
Bácsi K, Kósa JP, Lazáry Á, Horváth H, Balla B, Lakatos P, Speer G: A CYP3A7*1C-polimorfizmus hatása a csont ásványanyag-tartalmára posztmenopauzás nőkben, Orvosi Hetilap 2007;148(27):1273-80.
Book chapters:
Varga PP, Lazáry Á. A gerinc degeneratív megbetegedései [Spinal degenerative disorders]. In: Szendrői M: Ortopédia, egyetemi tankönyv, Semmelweis Kiadó, 2018. in press
Rónai M, Lazáry Á, Varga PP. A gerinc és a keresztcsont daganatos betegségeinek műtéti kezelése [Surgical treatment of the spinal and sacral tumors]. In: Szendrői M, Fekete K: Mozgásszervi sebészeti műtéttan, Medicina Kiadó, Budapest, 2018. in press
Klemencsics I, Lazáry Á, Varga PP. Spinális infekciók műtéti kezelése [Treatment of spinal infections]. In: Szendrői M, Fekete K: Mozgásszervi sebészeti műtéttan, Medicina Kiadó, Budapest, in press
Varga PP, Jakab G, Lazáry Á. Degeneratív thoracolumbális gerincebészet [Degenerative thoracolumbar spine surgery]. In: Szendrői M, Fekete K: Mozgásszervi sebészeti műtéttan, Medicina Kiadó, Budapest, in press
Varga PP, Jakab G, Szöverfi Z, Bors I, Lazary A. Percutaneous cement discoplasty: minimally invasive treatment of severe disc degeneration in elderly. In: Lewandrowski KU. Minimally Invasive Spinal Surgery. JP Medical Publishers, 2018.
Varga PP, Szövérfi Z, Lazáry Á. Csigolyát és sacrumot érintő lágyrészsarcomák [Soft tissue sarcomas of vertebrae and sacrum]. In: Szendrői M: Malignus lágyrésztumorok diagnosztikája és kezelése. Medicina Kiadó, Budapest, 2017.
Varga PP, Szövérfi Z, Lazáry Á. Sacrum resections and reconstructions. In: Aydinli U: Diagnosis and the Treatment of Spine and Spinal Cord Tumors. Turkish Spine Society. 2015
Varga PP, Szövérfi Zs, Lazáry Á: A gerinc és sacrum elsődleges és áttétes daganatai [Primary and secondary tumors of the spine and sacrum]. In: Szendrői M: Csont-, ízületi daganatok és daganatszerű elváltozások. Vol2, Medicina Kiadó, Budapest, 2015.
Varga PP, Lazáry Á: A patológiás csigolyatörések differenciáldiagnosztikája és korszerű sebészi kezelése [Differential diagnosis and modern treatment of pathological vertebral fractures]. In: Büki A, Szeifert Gy: A neurotraumatológia alapvonalai, Semmelweis Kiadó, Budapest, 2014.
T T Dao, P Pouletaut, F Charleux, Á Lazáry, P Eltes, P Pal Varga, MC Ho Ba Tho (2014) Estimation of Patient Specific Lumbar Spine Muscle Forces using Multi-Physical Musculoskeletal Model and Dynamic MRI In: V.-N. Huynh et al. (eds.), Knowledge and Systems Engineering, Volume 2, Advances in Intelligent and Soft Computing, Volume 245, 2014, pp 411-422.
Varga PP, Lazáry Á: Osteoporoticus gerinc műtéti kezelése [Surgical treatment of the osteoporotic spine]. In: A csontanyagcsere betegségei (szerk: Lakatos Péter, Takács István), Semmelweis Kiadó, Budapest 2012.
Lazary A, Varga PP. Clinical Use of Gypsum: Perspectives of Spinal Applications in Gypsum: Properties, Production and Applications, Editor: Delia H. Sampson, Nova Science Publisher 2010, (ISBN: 978-1-61728-308-6)
Invited lectures, podium presentations:
Treatment of spinal metastases. SEEFORT, Dubrovnik, 2017
Computational methods establish the future of spine surgery. VPHi Keynote webinar, 2017
3D szimuláció és nyomtatás a gerincsebészetben. Mindenki Akadémiája MTVA, Budapest, 2017
Osteoporotic spine characteristics. AOSpine Advanced Course, Budapest, 2013
Mechanobiology of the aging spinal segment. AOSpine Advanced Course, Budapest, 2013
Sacral pathologies in elderly. AOSpine Advanced Course, Budapest, 2013
State of the art in percutaneous vertebral augmentation: evidence in the debate. BBSpine, Budapest, 2013
Primary prevention of disc degeneration related symptoms. Spine Sciences’ State of the art forum, Geneva, 2013
Local recurrence and overall survival after surgical treatment of sacral chordoma – an analysis of prognostic variables from AOSpine Tumor Knowledge Forum Primary spinal tumor retrospective database. 11th International Turkish Spine Congress, Cesme, 2015
Lung cancer metastasis—the smart approach. AOSpine Davos Courses, Davos, 2017
Spinal cord compression due to metastatic renal cell carcinoma. AOSpine Davos Courses, Davos, 2017
Sacral chordoma—what’s on the horizon? AOSpine Davos Courses, Davos, 2017
3D szimuláció és nyomtatás a gerincsebészetben. IME Konferencia, Budapest, 2017
A lumbális csigolyaközti fúzió technikai evolúciója. Neurotrauma és Gerincsebészeti Tavaszi Szimpózium, Budapest, 2017
Natural Course of the Degenerative Deformity. AOSpine Advances Symposium—Deformed Spine, Budapest, 2011
Complications of sacral chordoma resections in elderly. BBSpine, Budapest, 2012
Biomechanics and mechanobiology of spine surgery: the role of computer simulations. First Joint Conference of From Medicine to Bionics, Budapest, 2016
Extreme rare multiplex tumor-like lesion. BMBSpine, Budapest, 2017
Primary Spinal Tumors. EMSOS, Budapest, 2017
Prevention of back pain. Eurospine, Liverpool, 2013
Why I use PMMA? Eurospine, Milan, 2016
Chordoma of the Sacrum, En Bloc Total Sacrectomy and Lumbopelvic Recontruction. Eurospine, Dublin, 2017
From in silico simulations to the operating table: new era in spine surgery. INSIGNEO showcase, Sheffield, 2016