A herniated disk refers to a problem with one of the rubbery cushions (disks) between the individual bones (vertebrae) that stack up to make your spine.
A spinal disk is a little like a jelly donut, with a softer center encased within a tougher exterior. Sometimes called a slipped disk or a ruptured disk, a herniated disk occurs when some of the softer “jelly” pushes out through a tear in the tougher exterior.
A herniated disk can irritate nearby nerves and result in pain, numbness or weakness in an arm or leg. On the other hand, many people experience no symptoms from a herniated disk. Most people who have a herniated disk don’t need surgery to correct the problem.
Symptoms
Most herniated disks occur in your lower back (lumbar spine), although they can also occur in your neck (cervical spine). The most common signs and symptoms of a herniated disk are:
Arm or leg pain. If your herniated disk is in your lower back, you’ll typically feel the most intense pain in your buttocks, thigh and calf. It may also involve part of the foot. If your herniated disk is in your neck, the pain will typically be most intense in the shoulder and arm. This pain may shoot into your arm or leg when you cough, sneeze or move your spine into certain positions.
Numbness or tingling. People who have a herniated disk often experience numbness or tingling in the body part served by the affected nerves.
Weakness. Muscles served by the affected nerves tend to weaken. This may cause you to stumble, or impair your ability to lift or hold items.
You also can have a herniated disk without knowing it — herniated disks sometimes show up on spinal images of people who have no symptoms of a disk problem.
When to see a doctor
Seek medical attention if your neck or back pain travels down your arm or leg, or if it’s accompanied by numbness, tingling or weakness. (Request an appointment with Dr. Lazary)
Causes
Disk herniation is most often the result of a gradual, aging-related wear and tear called disk degeneration. As you age, your spinal disks lose some of their water content. That makes them less flexible and more prone to tearing or rupturing with even a minor strain or twist.
Most people can’t pinpoint the exact cause of their herniated disk. Sometimes, using your back muscles instead of your leg and thigh muscles to lift large, heavy objects can lead to a herniated disk, as can twisting and turning while lifting. Rarely, a traumatic event such as a fall or a blow to the back can cause a herniated disk.
Risk factors
Factors that increase your risk of a herniated disk may include:
Weight. Excess body weight causes extra stress on the disks in your lower back.
Occupation. People with physically demanding jobs have a greater risk of back problems. Repetitive lifting, pulling, pushing, bending sideways and twisting also may increase your risk of a herniated disk.
Genetics. Some people inherit a predisposition to developing a herniated disk.
Complications
Your spinal cord doesn’t extend into the lower portion of your spinal canal. Just below your waist, the spinal cord separates into a group of long nerve roots (cauda equina) that resemble a horse’s tail. Rarely, disk herniation can compress the entire cauda equina. Emergency surgery may be required to avoid permanent weakness or paralysis.
Seek emergency medical attention if you have:
Worsening symptoms. Pain, numbness or weakness may increase to the point that you can’t perform your usual daily activities.
Bladder or bowel dysfunction. People who have cauda equina syndrome may become incontinent or have difficulty urinating even with a full bladder.
Saddle anesthesia. This progressive loss of sensation affects the areas that would touch a saddle — the inner thighs, back of legs and the area around the rectum.
Prevention
To help prevent a herniated disk:
Exercise. Strengthening the trunk muscles helps stabilize and support the spine.
Maintain good posture. Good posture reduces the pressure on your spine and disks. Keep your back straight and aligned, particularly when sitting for long periods. Lift heavy objects properly, making your legs — not your back — do most of the work.
Maintain a healthy weight. Excess weight puts more pressure on the spine and disks, making them more susceptible to herniation.
Treatment
Medications
Over-the-counter pain medications. If your pain is mild to moderate, your doctor may tell you to take an over-the-counter pain medication, such as ibuprofen (Advil, Motrin IB, others) or naproxen (Aleve, others).
Narcotics. If your pain doesn’t improve with over-the-counter medications, your doctor might prescribe narcotics, such as codeine or an oxycodone-acetaminophen combination (Percocet, OxyContin, others), for a short time. Sedation, nausea, confusion and constipation are possible side effects from these drugs.
Anticonvulsants. Drugs originally designed to control seizures also may be helpful in the treatment of the radiating nerve pain often associated with a herniated disk.
Muscle relaxers. Muscle relaxants may be prescribed if you have muscle spasms. Sedation and dizziness are common side effects of these medications.
Cortisone injections. Inflammation-suppressing corticosteroids may be given by injection directly into the area around the spinal nerves. Spinal imaging can help guide the needle more safely. Occasionally a course of oral steroids may be tried to reduce swelling and inflammation.
Physical Therapy
If your pain has not resolved within a few weeks, your doctor may suggest physical therapy. Physical therapists can show you positions and exercises designed to minimize the pain of a herniated disk.
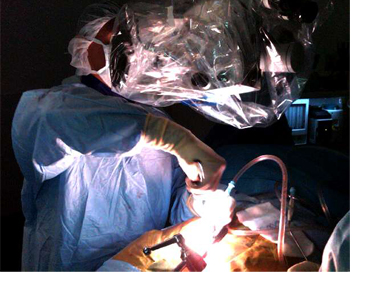
Surgery
A very small number of people with herniated disks eventually need surgery. Your doctor may suggest surgery if conservative treatments fail to improve your symptoms after four-six weeks, especially if you continue to experience:
Numbness or weakness
Difficulty standing or walking
Loss of bladder or bowel control
In many cases, surgeons can remove just the protruding portion of the disk (microdiscectomy). Rarely, however, the entire disk must be removed. In these cases, the vertebrae may need to be fused together with metal hardware to provide spinal stability (spinal fusion). Rarely, your surgeon may suggest the implantation of an artificial disk (artificial disc replacement).

Cost of a spine surgery
Real cost of a spine surgery is dependent from the type of the surgery, the need for implants, the length of hospital stay. The variety in countries, the travel and accommodation costs highly influence the total expenses related to the surgical treatment of different...
SPINE SURGERY IN BUDAPEST
A number of health care providers offer different solutions for spinal surgeries all over the world. The diversity of quality and costs is very high even inside Europe. On the other hand, health tourism is more and more popular and patients seek for safe and high...

Spine surgical consultation during the pandemic
Our private spine surgical consultation and spine care service is running in the Buda Health Center according to the relevant regulation. Examination and treatment are performed in accordance with the decree of the government. Safety of patients and health care...

Comprehensive spine surgery
Modern spine care is the effective and safe combination of evidence-based diagnostic and surgical techniques and different patient-specific solutions providing the best outcome for the patients. Highly educated spine surgeons use modern, safe diagnostic tools to find...

Minimally Invasive Surgery
In general, the goal of minimally invasive spine surgery (MIS) is to stabilize the vertebral bones and spinal joints and/or relieve pressure being applied to the spinal nerves — often a result of conditions such as a spinal instability, bone spurs, herniated discs,...
